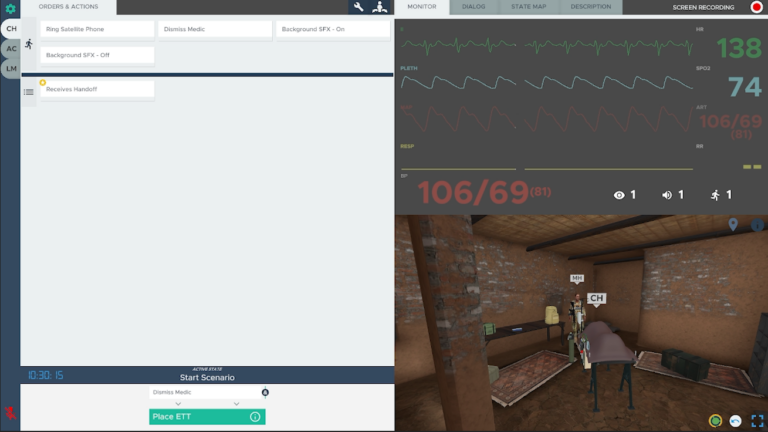
Case Description
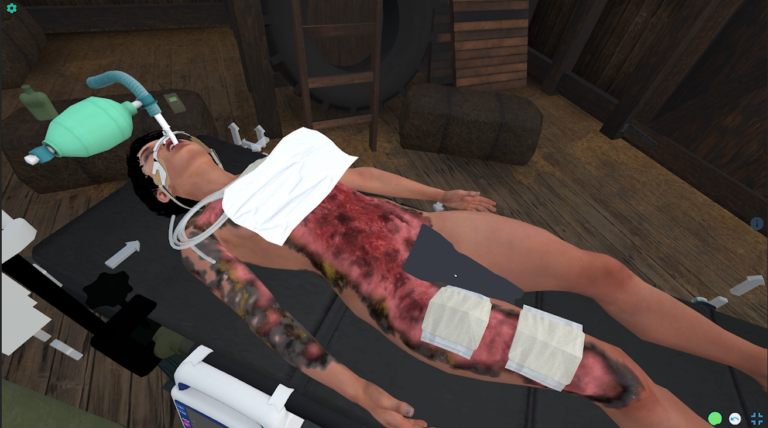
Starting in a building of opportunity in a far forward location, participants receive handoff for a casualty that suffered severe TBI and blast injury including bilateral lower extremity amputations. The learner should assess the patient, initially recognizing that the cric placed in the field is a false passage. They should place an ETT and put the patient on the ventilator. Patient also has a proptotic eye, indicating retrobulbar hematoma, and the learner should perform a lateral canthotomy. Amputations should be dressed with hemostatic gauze and pressure dressings, and the tourniquets relaxed. Learners should perform PCC nursing measures. As the case progresses, the patient develops hypotension and a positive FAST exam. Learners should give TXA and blood. As the case progresses further, the patient will develop signs of brain herniation. Despite heroic efforts, the casualty will succumb to their injuries. The learners should identify grave prognosis and provide palliative care.
When starting the scenario, there is an option to add a second or third patient to the scenario for additional complexity for advanced teams.
Learning Objectives
1. Demonstrate ability to provide patient care for extended periods of time when evacuation or mission requirements surpass available capabilities and/or capacity to provide that care.
2. Understand the use of the MARC2H3-PAWS-L algorithm in prolonged casualty care.
a. Evaluate for massive hemorrhage, and appropriately manage resources during a massive casualty situation.
b. Evaluate airway patency and perform interventions if indicated.
c. Evaluate respirations and perform any indicated interventions.
d. Evaluate circulation, and if required give IV fluids or blood products to improve circulation. Consider conversion of tourniquets placed in the field.
e. Communicate appropriately with the casualty, team members, tactical leadership, evacuation platform, logistics support, and perform teleconsultation.
f. Prevent hypothermia, and manage hyperthermia.
g. Evaluate for head Injury and if identified perform serial neurologic checks and appropriate treatments to mitigate the effects of increased intracranial pressure from traumatic brain injury.
h. Provide appropriate pain control.
i. Give antibiotics as indicated.
j. Evaluate for wounds or burns and place appropriate dressings. Provide appropriate nursing care to keep wound dressings clean.
k. Provide appropriate splinting if indicated.
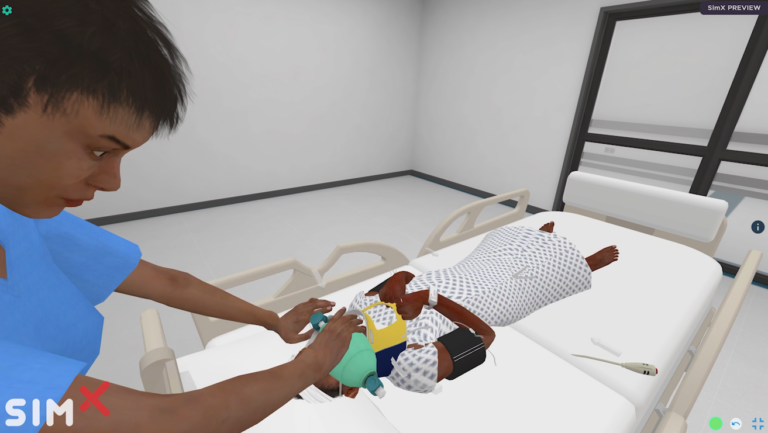
3. Understand the essential PCC capabilities – monitor, resuscitate, ventilate/oxygenate, airway control, sedation/analgesia, physical exam, diagnostics, nursing and hygiene, surgical interventions, telemedical consult, and package and prepare for flight.
4. Identify that cricothyrotomy placed in the field is not ventilating the patient, and perform endotracheal intubation.
5. Diagnose retrobulbar hematoma based on clinical exam of proptosis and unresponsive pupil, and perform immediate lateral canthotomy.
6. Identify decompensation and repeat MARCH assessment. Identify intra-abdominal hemorrhage and manage appropriately with blood resuscitation.
7. Identify progressive TBI and concern for impending herniation, manage appropriately with head elevation, hypertonic solution, and teleconsultation.
8. Recognize grave prognosis with likely completed brain herniation and provide palliative care measures.
MINIMUM:
OS: Windows 10
Processor: Intel Core i5-2300 | AMD FX-4350
Memory: 4 GB RAM
Graphics: Nvidia GeForce GTX 2060
DirectX: Version 11
Storage: 12 GB available space
RECOMMENDED:
OS: Windows 10
Processor: Intel Core i7-2300 | AMD FX-4350
Memory: 8 GB RAM
Graphics: Nvidia GeForce GTX 3060
DirectX: Version 11
Storage: 12 GB available space
Interested in this scenario?
Sign up to talk with a member of the SimX team today!