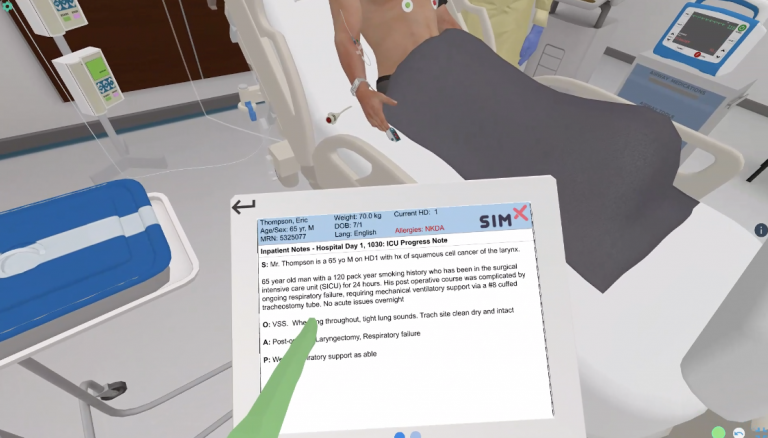
The patient is a 65 year-old man who has been in the MICU for 14 days with acute respiratory distress syndrome (ARDS). He had a percutaneous tracheostomy performed two days ago and he continues to require mechanical ventilatory support. You are called to the bedside by the ICU nurse because the ventilator’s high pressure alarm is going off and the patient is becoming hypoxic. The nurse states that this happened immediately after completion of a portable chest x-ray.
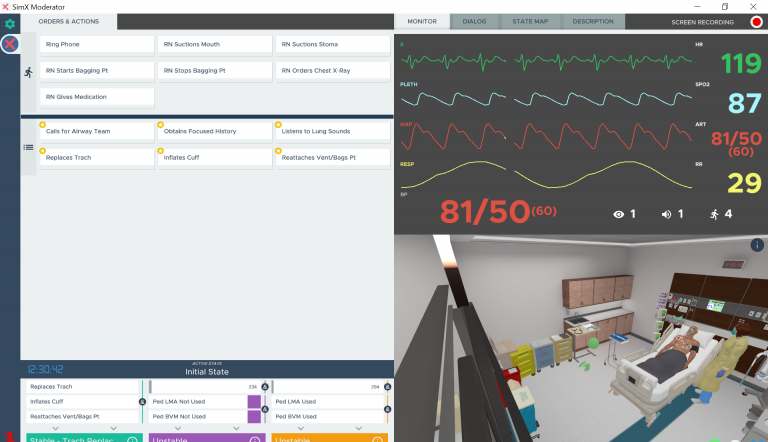
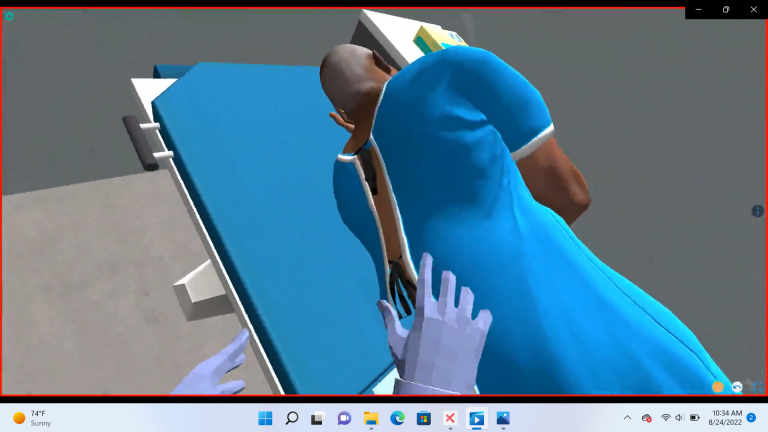
The patient will initially be in respiratory distress and then will develop progressive hemodynamic instability and worsening hypoxemia. The learner should assess the patient and diagnose and manage tracheostomy displacement and tension pneumothorax.
The learner should re-intubate with an endotracheal tube. After intubation, the patient’s hypoxia will improve, but will develop hypotension and tachycardia. This should prompt the learner to continue their assessment, and, with ultrasound and/or portable chest x-ray, diagnose tension pneumothorax. This is ultimately relieved when needle decompression is performed and/or a chest tube is inserted.
Learning Objectives
– Determine why a tracheostomy was performed, when it was performed, and the type of tracheostomy tube in place
– Diagnose that the tracheostomy tube is no longer in the trachea and has entered a false passage
– Understand the difference in management of displacement of acute versus chronic tracheostomy tubes
– Demonstrate appropriate management of tracheostomy tube displacement and tension pneumothorax
MINIMUM:
OS: Windows 10
Processor: Intel Core i5-2300 | AMD FX-4350
Memory: 4 GB RAM
Graphics: Nvidia GeForce GTX 2060
DirectX: Version 11
Storage: 12 GB available space
RECOMMENDED:
OS: Windows 10
Processor: Intel Core i7-2300 | AMD FX-4350
Memory: 8 GB RAM
Graphics: Nvidia GeForce GTX 3060
DirectX: Version 11
Storage: 12 GB available space
Interested in this scenario?
Sign up to talk with a member of the SimX team today!